Special Programs - Pulmonary and Critical Care Medicine Fellowship
Multi-Institutional Education Programs
Our fellowship program at the University of Maryland provides leadership and participation in a Multi-Institutional Education Program in the Mid-Atlantic region. Pulmonary/Critical Care and Critical Care Fellowship Programs from 7 institutions (University of Maryland, NIH Clinical Center, Washington Hospital Center, Georgetown University, George Washington University, Johns Hopkins Hospital, and Walter Reed National Military Medical Center) currently participate in these educational courses, and the University of Maryland is one of the primary sites for leadership coordination and educational activities.
This education curriculum currently consists of two annual blocks of educational coursework. The first is the Introductory Course in Pulmonary and Critical Care Medicine for three weeks in July of each year. At the University of Maryland, all of our first year fellows participate in this course prior to the start of clinical rotations, and thus there are no clinical responsibilities for fellows during this time. The second is the Intermediate and Advanced Course in Pulmonary and Critical Care Medicine for two weeks in January/February of each year. Topics for both the July and January courses are determined by the course directors, and generally are included within the broad categories of Mechanical Ventilation, Evidence Based Medicine, Ultrasound, Pulmonary Medicine, Critical Care Medicine, Radiology, Physiology, and Procedures. Educational responsibilities are shared among the seven institutions and the core subjects are presented by faculty from these institutions. The educational program consists of lecture material presented in a didactic manner, and the lectures are reinforced by practical demonstrations, small group exercises and simulations during both the Introductory and Advanced courses.
Fellows have expressed high levels of satisfaction with the organization and perceived value of this educational program, with the overwhelming majority of fellows from our Fellowship and the other institutions indicating that this program is a very valuable component of their fellowship training. The collaboration among multiple institutions allows us at Maryland to pool faculty resources and expertise to provide a comprehensive educational experience for all our fellows throughout their fellowship training.
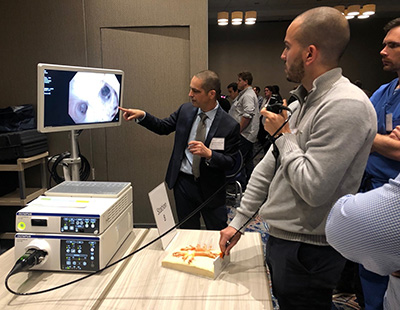
Bronchoscopy

Our Pulmonary and Critical Care Division at the University of Maryland has had a long-standing reputation for experience and expertise in the areas of diagnostic and interventional bronchoscopy. Our current bronchoscopy suite has state-of-the art video bronchoscopy equipment, monitoring technology, and a dedicated fluoroscopic C-arm. The Division performs over 1000 bronchoscopy procedures each year at UMMC, and approximately 100 yearly at the VA. Our large volumes enable fellows to become proficient in all aspects of diagnostic bronchoscopy, and to gain exposure and experience with all aspects of interventional bronchoscopy.
A particular focus of our Division for many years has been diagnostic and staging transbronchial needle aspiration (TBNA).Bronchoscopy with endobronchial ultrasound (EBUS) as a diagnostic and staging tool has become a standard, routine procedure within our Division. Fellows have numerous opportunities to develop proficiency with EBUS throughout their fellowship training.
The Interventional Pulmonology (IP) program at UMMC is an integral part of our Division. The IP program offers a complete array of diagnostic, therapeutic, and palliative airway procedures, including bronchial thermoplasty, electromagnetic navigation bronchoscopy, rigid bronchoscopy, PDT, LASER therapy, APC, cryotherapy, and stenting. The IP service is also very active in the management of patients with pleural disease, with expertise in thoracic ultrasound guided assessment and interventions of the pleural space, pleurodesis, pleural catheter placement (chest tube, small bore catheter, and tunneled pleural catheter), pleural manometry, and closed pleural biopsies. Our fellows have numerous opportunities to gain exposure and experience within the realm of IP. These opportunities and interactions occur as the fellow rotates on many inpatient and outpatient rotations at UMMC, Midtown, and VA, or by the fellow rotating on the IP service. Although it is not possible for a pulmonary/critical care fellow to become proficient in all areas of IP during a 3 year combined fellowship, the numerous opportunities for exposure and experience with all aspects of diagnostic and interventional bronchoscopy allow each fellow to develop a very good understanding of the field and to make well-informed decisions about their areas of interest in their future careers.
Simulation Center
The MASTRI Center (Maryland Advanced Simulation, Training, Research and Innovation) at the University of Maryland is an innovative, research-driven, high-technology, state-of-the-art training center. Its goals are to lead in evaluation, development, and testing emerging simulation technologies and techniques and in the ongoing transformation of surgery and other medical procedures. Additionally, the Center is envisioned as a premier educational environment devoted to the training of healthcare practitioners across a diverse spectrum, with focus on how users learn and adapt to new technologies.
Our pulmonary fellows have the opportunity to participate in simulation models for diagnostic bronchoscopy (including simulation of forceps biopsy and TBNA), endobronchial ultrasound (EBUS), chest tube insertion, and use of video laryngoscopy as an intubation technique. The bronchoscopy simulation software is a major learning tool for the fellows as they develop proficiency with this procedure. In addition, the fellows participate in a longitudinal simulation curriculum with sessions through the year.
Trauma Anesthesia Rotation
Trauma Anesthesiology is a section of the Maryland R Adams Cowley Shock Trauma Center. This section performs more than 6,000 intubations each year and is the only group of anesthesiologists in the country with a practice focused specifically on traumatic injury. The section trains numerous residents each year rotating in one-month blocks from multiple institutions in the Mid-Atlantic region. For our fellowship, this one-month rotation is an elective rotation for 3rd year fellows
During this rotation, the fellow learns advanced airway management skills under the direct supervision of a Trauma Anesthesiologist. Most of our fellows who have participated in this rotation have performed 50-60 intubations either in the operating room or in the Trauma Resuscitation Unit. Fellows and practicing clinicians in pulmonary and critical care medicine are increasingly expected to have substantial proficiency in endotracheal intubation and airway management. This rotation expands upon airway management skills developed during the Critical Care Anesthesia rotation.
Sleep Medicine
The Sleep Disorders Center at the University of Maryland is a multidisciplinary center performing comprehensive clinical and laboratory evaluation of patients with a variety of sleep disorders. Under the direction of Steven Scharf, MD, a member of our Division and a board-certified pulmonary and sleep specialist, specialists from diverse fields including ENT, Psychiatry, Dentistry, Neurology and Pediatrics, evaluate and manage a wide variety of pulmonary and non-pulmonary sleep disorders. The center maintains an outpatient clinic and a sleep laboratory. Fellows have the opportunity to rotate through the outpatient sleep center, engage in research projects linked to sleep disorders and develop clinical skills necessary for the management of sleep-disordered breathing within the framework of a pulmonary medicine practice.
